Blood supply
The blood supply to the mammary gland is extremely important for mammary function. All of the milk precursors come from blood. To produce 1 liter of milk 500 liters of blood have to pass through the udder. When a cow produces 60 liters of milk per day, 30,000 liters of blood are circulation through the mammary gland. This represents a blood flow of 1250 liters per hour.
There is a 2-6 fold increase in blood flow in the mammary gland starting 2-3 days prepartum. The decrease in production with advancing lactation is not due to decreased blood flow, rather it is due to the loss of secretory epithelial cells through a process programmed cell death, this process is called apoptosis.
Arterial system
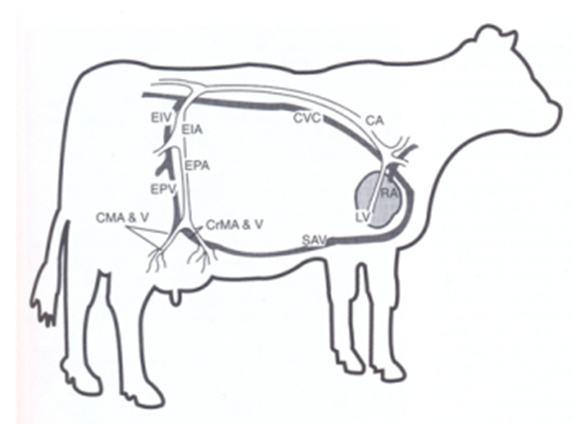
Blood leaves the heart and flows towards the rear of the cow by the abdominal aorta (Figure 5). Two major arteries carry the blood to the udder, on for each half of the udder. These arteries, pudendal arteries, enter the udder through the inguinal canal. The inguinal canal is the orifice in the body cavity in the inguinal region where blood vessels, lymph vessels and nerves enter and leave the body cavity to supply the skin in the posterior part of the animal. The pudendal arteries are branches of the external iliac arteries, which are branches of the abdominal aorta. The external iliac artery becomes the femoral artery (supplies leg muscles). The external pudendal arteries become the mammary arteries as mentioned above pass through the inguinal canal. The mammary arteries divide into caudal and cranial branches, which rebranch many times and end in small capillaries surrounding each alveolus. The pudendal arteries make S-shaped curves (sigmoid flexures) as they emerge from the inguinal canal. This allows for downward distension of the udder as it fills with milk, without stressing the blood vessels. Perineal arteries supply blood to a small portion of the posterior dorsal part of the udder.
 Information[1]
Information[1]RA= right atrium | LV= left ventricle | CA= caudal aorta | CVC= caudal vena cava |
EIV= external iliac vein | EIA= external iliac artery | EPA= external pudendal artery | EPV= external pudendal vein |
CMA&V= caudal mammary artery and vein | CrMA&V= cranial mammary artery and vein | SAV= subcutaneous abdominal vein |
Venous system
Veins leave the mammary gland anti-parallel to the arteries. There are three veins on each side that carry blood away from the gland:
External pudendal vein leaves the udder parallel to the external pudendal arteries;
Subcutaneous abdominal vein (milk vein) exits the gland at the anterior end of the front quarters and passes along abdominal wall. This is the large vein that is visible under the skin on the belly of the cow. It enters the body cavity at the xiphoid process via "milk wells", and eventually empties into vena cava.
Perineal vein leaves the rear of the gland parallel to the perineal artery and carries less than 10% of blood leaving udder.
Venous circle
Venous circle is formed by anastomoses between anterior and posterior mammary veins. It prevents pinching off of areas of venous outflow when the cow is lying down.
Lymphatic system
The lymphatic system carries lymph from the tissues toward the heart. Because many molecules of all sizes leave the capillaries but not all return to the venous blood drainage at the tissue level. Especially the larger molecules like proteins. These, along with cellular metabolites and some secretory products are in the interstitial (extracellular) spaces. If they stayed there, they would disrupt with the normal balance of osmotic pressure in the tissue, upsetting trans-capillary fluid exchange. Excess fluid (called extracellular fluid) would accumulate in the interstitial spaces. The lymph is drained toward the upper posterior part of the udder, where they converge on the convex surface of the supramammary lymph node.
Functions of lymphatic system:
The extracellular fluids are drained from the tissue and conducted back to the circulatory system via the lymphatic network;
Also, the lymphatics contain concentrated areas of leukocytes (particularly lymphocytes and macrophages) in lymph nodes; these leukocytes can mount an immune response to bacteria and foreign material;
The lymphatic network serves to transport some elements in the body (vitamin K, lipids absorbed in the intestine).
Lymphatic network
Lymphatic network originates in tissue spaces as very thin, closed endothelial tubes (lymphatic capillaries). These are analogous to blood capillaries, but are much more permeable, with little resistance to passage. They have no basement membrane. Lymph capillaries converge to form larger vessels. Lymph flow is unidirectional from the tissues through lymphatic vessels, eventually dumping lymph into the vena cava.
Lymph is a clear, colorless liquid with a composition similar to blood plasma. Changes in plasma composition will change lymph composition. Protein concentration of lymph is lower than in plasma, 1.5% vs. 6%, respectively. Specific proteins differ, for example albumin is a smaller molecular size than globulins and leaves the capillaries more readily than globulins, so the albumin: globulin ratio is 1.8 in plasma, 2.5 in lymph. Protein concentration in lymph varies inversely with rate of formation.
Lymph flow rate is usually low. It is influenced primarily by the rate of lymph formation. For example, if blood capillary pressure is increased by arterial vasodilation or venous constriction, the flow rate of lymph increases. Also, the flow rate is affected by compression of lymphatics by contraction of neighboring musculature and by negative intrathoracic pressure (breathing). Valves in the lymph vessels prevent retrograde flow similar to those in veins.
Udder edema
Edema is swelling of the udder. Although it occurs to some degree in most cows at calving time, heifers calving for the first time are especially prone to having udder edema. Fluid accumulates between skin and glandular tissue, as well as in the gland. Severe edema can strain supportive structures of udder. Udder edema is often caused by an imbalance of hydrostatic and osmotic pressures, increasing fluid flow out of the capillaries into the interstitial spaces. This may occur because of damage to the capillary walls or obstruction of the lymphatic system.





